Good and Healthy Bones
 Tuesday, November 28, 2017 at 10:22PM
Tuesday, November 28, 2017 at 10:22PM What are GOOD BONES?
Bones that exhibit the proper marriage of bone structure and bone density together represent the true measure of healthy or Good Bones. Quality and Quantity. Healthy bones are not too rigid or too weak. Rigid bones could have high density but a poor bone structure and micro-cracks repair record. Low density bones also 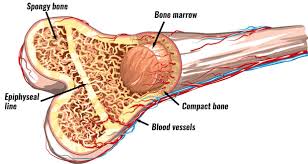 might be weak or not weak depending on these internal bone repair factors and sound structure. Good bones are able to give a little under stress like skyscrapers during earthquakes without cracking or breaking. A new bone Doctor article.
might be weak or not weak depending on these internal bone repair factors and sound structure. Good bones are able to give a little under stress like skyscrapers during earthquakes without cracking or breaking. A new bone Doctor article.
FYI: Scientists have for quite some time only found two things that significantly impact bone strength: 1. Weight bearing exercise to put torque on bones that tells them to get stronger. ref ref And 2. Consuming more fruits and vegetables. Very little calcium in those foods, but the more important minerals of potassium and magnesium (pH buffers) help protect the calcium that is already in the bones to stay there. Vitamins D3, K2 (ref), C, and E along with adequate protein also play vital roles in bone health. ref ref article
reference*** on how to maintain a lifetime of healthy bones. As the preceding referenced article mentions, calcium is just one of 10 factors to help bones. Plus, longer term bone studies have now revealed that taking extra calcium or even extra calcium with vitamin D has only limited success at preventing fractures, and at certain dosages, may have adverse effects instead. This fact should have initiated changes to bone health recommendations that included all 10 remedies mentioned. Indeed, measuring bone density, the hallmark of mainstream medicine for bone health, actually only represents a rather small percentage of bone fracture reduction. Take a moment for this to sink in. Yes, density is important, but mostly in an overall context with a sound bone structure.
***To complete these 10 ways to have healthy bones, here are another two nutrients that have to be included, plus the B complex vitamins are vital, especially B12. Vitamin B12 deficiency reduces bone building cell production. ref The B vitamins hopefully are included under #1, eat more vegetables, but need to be mentioned. The next two additions could fit with number 7 collagen. Vitamin C with protein manufacture body collagen while the active form of silicon directs collagen production and placement, especially for bone building and repair. ref
How did the calcium bone connection get started in the first place? Thank the Dairy Industry for this one. Early research studying milk effects on bones revealed that indeed bone density increased. From these short term studies, most only about a year long, it was assumed that this increased density would give bones future fracture prevention. ref And some studies showed such a connection in animal studies since animals have a shorter lifespan and this can be determined in a rather short time. Now after longer term human studies revealed this may not be the case, new theories need to be developed that explain why and what does support a lifetime of healthy bones. But, this has not exactly happened. Why not?
1. Some Scientific studies still weakly support the old theories.
2. Industries with their lobbyists have gained too much control over Government Health Agency Scientists, research decisions, and grant money?
3. Science is very slow to initiate changes to established dogma?
4. There are so many variables that studies can be developed to reveal opposite views?
5. To the many people who suffer from the 1.5 million bone fractures each year, this is potentially a critical life situation. And what about the opposite action on cardiovascular conditions? ref Shouldn't this issue be given top priority and factual study results be readily analyzed and available? MD article
Dogma, faulty science, special interests, and biased professionals should not be part of the solution for how to maintain healthy bones since they have so completely failed according to past statistics. You will have to become educated on your own to survive alive and save your bones. Look at what Harvard Medical is now saying about how much calcium is needed. here
Of Interest: Traditional mainstream medicine has lost touch with innate Body Wisdom for building strong bones. Consuming extra calcium is a lot like delivering extra bricks when building a fence. At first it looks like a good idea is working, but then there are only so many bricks that can be used to finish the fence.** Then the extra bricks just get in the way. More bricks does not help while more bricklayers could. The nutrients and actions that help calcium go to the right places and stay away from the undesirable areas may be important rather than just the amount of calcium. The body simply turns off absorption when extra calcium is consumed and increases absorption when less calcium is available from food. It is interesting to note that higher sodium from salt increased calcium urine content out of the body. But it also sparked an increase in calcium intake percentage during digestion that balanced the two amounts. What appears to rob calcium and eliminate it from the body is excess sugar, not salt. There are many avenues for this action. ref
**Bones are a little different than fences in that bones have to be light and flexible yet strong while a fence is heavy and strong. Fences that have decorative holes or open spaces in them are more like bones. Thus, the extra bricks could be used to fill in the holes up to a point. Bones use the open spaces to act as a reservoir for extra calcium for future use by the body, but not necessarily for overall greater bone strength once past that certain point.
Put on your Sherlock Holmes hat and using inductive reasoning, discover what is really happening. First, look up the meaning of inductive and how Sherlock used it to solve mysteries. Logically deductive reasoning must be what the early Scientist used when they assumed future bone fracture protection from short term milk studies showing increased bone density. Some body processes must not follow logically accepted patterns. Yes, Bones contain a lot of calcium. And denser bones often exhibit fewer fractures. But, people with low density bones can still have strong and low fracture rate bones if the macro-structure is solid and bone turnover mechanisms are operating normally.
With osteoporosis, more fat cells are generated in bone marrow than normal. Why do bone marrow stem cells change the balance to more fat cell production instead of equal bone building cell production? ref
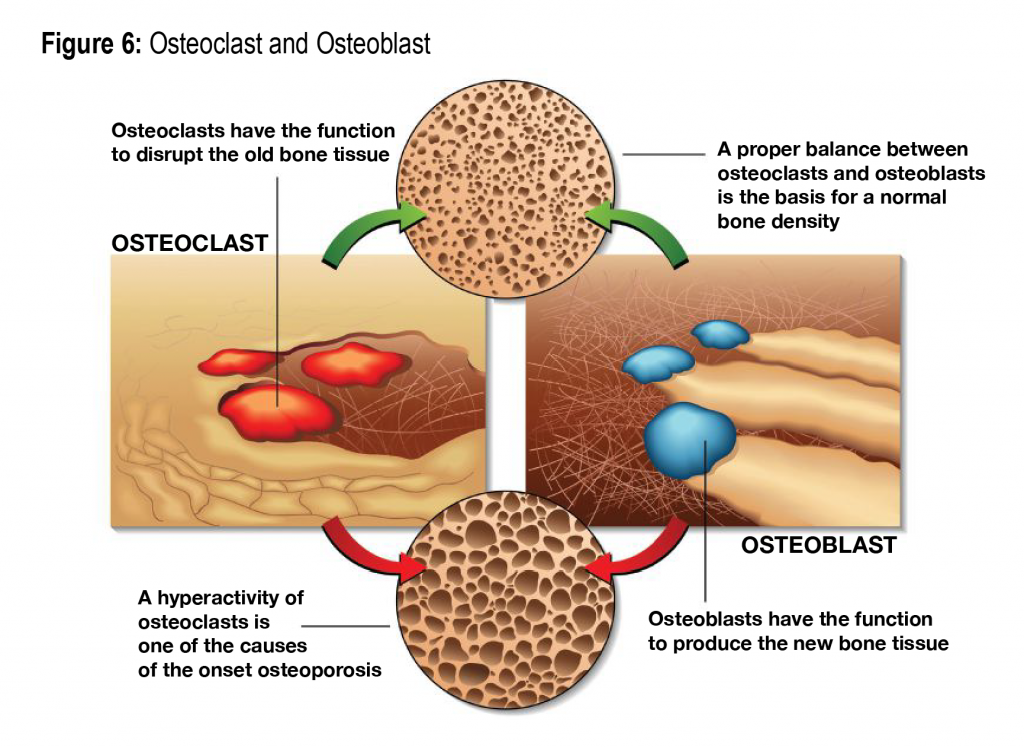
OSTEOPOROSIS is a condition of disrupted bone repair and renewal rather than just a low calcium condition. Oats help, ref <Very important reference. Add this one too on vitamin K2.
Definition: Cancellous bone is the spongy honeycomb like bone making up the pelvis, backbone vertebrae, and inside the end tips of long bones. Cortical bone tissue forms the shaft of long round bones and also it forms a protective layer surrounding the spongy bones. Because cortical bone is compact, it represents about 80% of bone even though it looks like a smaller amount of bone. Osteoporosis largely effects the cancellous bone tissue due to its honeycomb form getting easily weakened, but cortical bone replacement can suffer as well. Cancellous bone tissue also is found inside the long bones housing the bone marrow where blood cells are produced. Apoptosis is the normal timely death of cells. ref In the study referenced above, scientists disrupted the normal death of bone building cells to get them to survive longer and while this did increase bone density, the bone exhibited greater porosity and weakness. Osteocytes are osteoblast cells that did not die and moved from the surface building of bone tissue into the middle of the bone to perform other bone repair processes, especially stress strain cracks. Osteocytes regulate RANKL production for the generation of bone tearing down cells, the osteoclasts. ref RankL, RANK, and OPG regulate the rate of bone turnover for healthy bone. If old bone cells building are not replaced, the old cells are not able to keep up with the demands and bones become porous.
FACT: People in Countries that consume less than half the amount of calcium consumed in the United States often exhibit far fewer bone fractures. Their bone micro structure probably is better organized and thus bones are stronger. Plus, the overall diet and activity level probably protect the lower calcium diets by holding onto bone calcium more effectively. See Magnesium and Bone integrity below.
This very important reference from above report highlights what the Scientists discovered is happening inside bones that increase fracture risk. In a nutshell; the lifespan of bone cells is disrupted. OLD BONE TISSUE IS NOT GETTING PROPERLY REPLACED AND CRACKS ARE NOT GETTING REPAIRED IN A TIMELY MANNER. The resulting porous condition weakens bones and increases fracture risk. Adding just calcium and vitamin D at this point only has very limited fracture prevention abilities, and may actually interfere with proper bone repair. It more or less just adds a little density to the weakened bone structure already present. Mature built bone cells have space to pack in more calcium but this will not impact the underpinnings of the disrupted bone building replace and repair process. Bone drugs have influence on this process usually by destroying some of the bone tearing down cells to slow bone loss. Bone building factors are still needed as supplements to facilitate the little bone renewing or turnover still occurring. 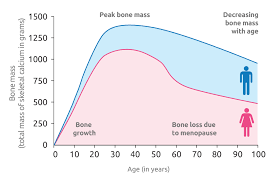
CALCIUM ROCKS BODY PROCESSES
Calcium is needed for many body functions plus it helps give bones a strong structure to anchor muscles. ref The calcium in bones can also serve another vital function for the body. If blood levels of calcium fall below a set point, the bones act as a reservoir to provide calcium into the blood. Calcium is needed in the blood at a certain level to allow muscles to contract and nerves to fire, plus numerous other important processes. Here is one of many ways the body can maintain this blood calcium level. Calcium from food is critical here. If not enough calcium is available, bone tissue can be broken down by vitamin D acting with the hormone PTH to release calcium into the blood. Vitamin D and PTH also increase calcium absorption from food and prevent calcium elimination out of the body. When the proper calcium amount in blood is attained, a thyroid hormone stops PTH and vitamin D actions and begins to put calcium back into bone tissue as well as prevent the extra absorption from food while increasing calcium elimination channels. These actions result in a very small but constant seesaw action on blood calcium levels which helps bone turnover for new bone repair and replace and to build up the bone calcium reservoir. The tips of long bones act as one of the reservoir sites. They can be filled or almost empty. Thus, depending upon how much of this reservoir bone calcium has been used, bone densities can fluctuate. Therefore, bone density does not always correlate with fracture prevention since it is at the middle of long bones that breaks occur and only sometimes at the tips. Measurements of bone turnover markers are necessary to know as vital factors for bone health.
IMPORTANT ASPECT: Bones act as mineral reservoirs and minerals can be taken out of bones for many body processes if the diet is short on supplying these minerals to blood plasma. One obvious use of calcium and magnesium from bone is to neutralize metabolic acids. The body would rather use potassium from fruits and vegetables, but will use calcium and magnesium when potassium is low. Potassium in the average diet is generally short of recommended amount (4700 mg) by about 40%. Did you notice that potassium is needed in the diet at an amount 4X greater than calcium (1200 mg)?
NOTE: Potassium requirement was recently reduced by US Government about 25% since so few people achieved anywhere near the 4700 mg mark. And government meal food programs were not able to easily meet that requirement for 1/3 daily requirement per meal. ref
VITAL POINT: Other body processes like acid regulation take priority over the use of bone minerals for integrity and strength of bones. Do you now see why fruits and vegetables are so vital for bone health? And they are just one of two major known bone protecting factors since they supply acid neutralizing minerals. Calcium is in second place to potassium by amount needed daily, but both have vital roles to play in the body. Calcium and magnesium act together as counterbalance actions for energy potential, such as muscle contraction. Magnesium has 299 other vital functions. Potassium is needed as a sister nutrient to sodium for water balance and nerve conduction, besides being the favorite mineral to neutralize body acids.
DETERMINING CALCIUM NEEDS
The preceding description is a large part of the criteria used by Scientists to determine how much calcium should be in the daily diet. The diet ideally should supply enough calcium to cover what is eliminated out of the body on a regular basis.** This is referred to as calcium balance or calcium homeostasis. This amount can vary widely and is influenced by many factors. Studies have shown a 200 mg to 700 mg daily spread. The average is about 300 mg. Since the absorption of dietary calcium averages 35%, regardless of source, a daily intake of 900 mg would cover so Scientists added 100mg buffer for the 1000mg recommendation. A new analysis reference revealed a calcium balance point at 741 mg per day, lower than expected. This measures calcium intake versus output. The body adapts to many factors to hold on to calcium if needed so lower amounts can still be adequate. Remember to determine calcium intake to add food sources and supplement amounts together.
Phosphate and Calcium
Calcium and phosphates have an important role to play separately and together in the body. They are needed within certain ratios of each other for harmony, although the Kidneys play a balancing role. Certain foods like colas have far to much phosphate similar to how dairy has too much calcium and luckily also some phosphate. ref
Potassium and Calcium
Another very important determinant is the amount of potassium in the diet. Why? The body would rather use potassium as the nutrient to neutralize normal acid build up in cells and blood plasma. ref If not enough potassium is consumed or available, calcium and magnesium will be called into action for this purpose. ref This would rapidly deplete these minerals in the blood and body cells so the process described above of removing calcium and magnesium from bones could come into play. A very expensive body process.
Magnesium and Calcium
This next concept is of immense significance. When magnesium intake is below recommended amounts (or too much above), which could also be a factor of excess calcium, or calcium magnesium balance, bone does NOT form properly. Plus, bone turnover is enhanced. This generates flaws in new bone structure, especially the bone meshwork. There is too much calcium mineralization and not enough magnesium in newly formed bone. ref Thus, even though this new bone would measure normal or higher in density, it is of a poor design which would fracture under less stress. ref
OTHER CRITICAL FACTORS IN BONE FRACTURE PREVENTION
Bone density is stepping aside. Bone turnover rate and the bone stress damage repair process are vital. This involves bone building cells called osteoblasts and bone tearing down cells called osteoclasts working in tandem to repair any micro-cracks as well as their work of consistent regeneration of small sections of old bone replaced with new bone, called bone turnover. New bone and old bone might have the same density, but new bone is stronger. another reason bone density measurements do not reveal the whole story. This bone turnover rate is a constant process throughout life, or at least it should be. For some reason, in osteoporosis, the bone building cells are not holding up their end of this process. The bone tearing down cells are still working and clearing out small sections of old bone, but the limited bone building cells are not able to keep up. More holes remain open causing bones to get porous and weak.
Determining Vitamins D and K2 needs
There are 2 different forms of Vitamin D. The storage low activity form that is increased by sunshine and diet, this is the one measured by Doctors, and the hormone form triggered by low calcium levels in blood and produced by Kidneys. The hormone form helps pull in calcium from food in the digestive tract, and if needed, it also tells bone tearing down cells to release calcium from bone. The storage form was thought to be neutral here, but, new information now reveals that the storage form gets involved in a novel way to protect bone mineralization. It goes into bone building cells and with the help of an enzyme, it turns into the hormone form and helps regulate the bone remodelling process directly. A certain level of the storage vitamin D is needed to be effective for this function. The effective amount of storage form vitamin D from animal studies puts it at 30 ng/mL.
NOTE: This reference expands some vitamin D forms and functions, note especially chart with VDR, vitamin D receptor involvement. There may be a new role for a rapid response action for some of vitamin D influence, since waiting for VDR gene activation would be too slow to explain some observations.
To get to 30 ng/ml, if starting at 15 ng/mL, it would be necessary to take a supplement of 1500 IUs for 3 months. There are factors that modify this amount. Have levels checked and work with a Nutritionist or Doctor. Plus, it is important that calcium ends up in bones and not soft tissues. Vitamin K2 helps here. the next reference is a study on fractures from low energy stress in children where calcium was not an issue, but K deficiency. ref
Vitamin K2
Vitamin K, both K1 and K2, have vital functions in the body. Vitamin K2 forms are necessary to compliment vitamin D for proper activation of osteocalcin which vitamin D helps form into the carboxylated conditon which binds with bone minerals and deposits them into and builds new bone tissues. But, since the two osteocalcin forms, uncarboxylated and carboxylated, have other body functions, like blood sugar control, it is necessary to keep vitamin K2 levels at amounts that will not upset the balance needed between the two osteocalcin forms. Thus, the prpper amount of vitamin K2 needed is still not adequately determined yet. But may be about 100 mcg for the MK7 form of vitamin K2. It all depends upon the percentage of osteocalcin that is carboxyated.
FYI: Doctors have been measuring the amount of carboxylated osteocalcin for quite some time. This shows them the status of bone building potential.
Of course, there are many moving parts to this bone turnover process where something could go awry. Dietary nutrients, hormones, glandular secretions, genetics, sunshine, and even exercise activities all play roles.
NOTE: Comprehensive review of many Vitamin D and Calcium studies by US Government. Quite technical.
THE COLLAGEN STRUCTURES
While calcium and vitamin D are important for generating bone density, equally as important or perhaps somewhat more is the structure of bone made up of collagen fibers laid down in layers, a lamination process. Collagen type 1 is built in bone building cells called osteoblasts. These are most of the vital nutrients needed for the production of strong collagen fibers; Vitamin C (ref), silica, protein building blocks called amino acids, manganese, copper, zinc, and vitamin K2. Vitamin D plays two roles with collagen. One is to assist with bone collagen while the other inhibits collagen in other cell types, like arteries, Kidneys, Lung, and Liver. Inhibiting certain collagen fibers in this case helps prevent cardiovascular and other fibrotic type diseases.
Only consuming calcium or even calcium with vitamin D misses the mark for complete strong bones. In fact, this might actually increase certain disease conditions when calcium turns up in places it does not belong, like in brain lesions as well as in artery wall plaque. ref All the following factors act as a team to first generate collagen bone structures, and then the minerals calcium, phosphorus, magnesium, and zinc fill up the structure to give strength from density but still retain a little flexibility so bones will not fracture under stress. When muscle action pulls on attached bones, this stimulates the process to build stronger bones.
Vitamins A and E and Essential fatty acids play indirect roles for bone health. Plus, these and other nutrients with anti-inflammatory elements also aid bone formation, repair, and maintenance.
For further info, read this article)
Clarification NOTE for Bone research: This may or may not be a factor to consider. Quite a few bone studies are conducted using mice or rats. Both of these animals make their own vitamin C, while humans do not. This fact could significantly influence bone factors and impact results. The results in humans could be very different from those in mice and rats for certain processes. Vitamin C is a factor in bone health. It is very much involved in building with proteins the collagen matrix upon which minerals are deposited. Plus, Vitamin C hinders osteoclasts (bone-destroying cells) while it stimulates the production of osteoblasts (bone-building cells). Thus, vitamin C promotes a healthy bone renewal rate. This would help prevent fractures. What is not known is how much vitamin C is being produced in the animal bodies during the tests or the level of vitamin C in humans for comparison.
BackGround Basics for Bone on Vitamins
Many of the concepts presented in the articles on this Website need to be tempered with the knowledge that some or many of the conditions mentioned may only happen on a tiny scale or to just small degrees of disruption to body functions. A major vitamin toxic conditon does not need to be present. It may take years for observable dysfunction to be revealed if at all. Most do unnoticed for so long that it is difficult to even be related back to the vitamin connections discussed. Even though major conditions do not develop, small errors over time can also lead to weaker bones. Bone fractions could also end up damaging artery walls to slowly limit flexibility of vessels. The recommendations are to be used as precautionary modes of prevention to maintain status quo and good health without noticeable disruptions to normal body metabolism.